Cognitive Behavioural Therapy (CBT) Explained: Your Complete Guide
In the pursuit of mental well-being, understanding the tools available is paramount. Cognitive Behavioural Therapy (CBT) stands as a cornerstone in modern psychotherapy, offering a structured and evidence-based approach to addressing a wide spectrum of mental health conditions. Its efficacy is widely recognized, with nearly 2 million CBT appointments taking place across England in 2021 alone, marking a significant increase in its utilization. Curio Counselling Calgary practices use of CBT therapy to help experience meaningful and lasting change that allows them to heal, grow, and thrive in all areas of their lives.
What This Guide Will Cover
This comprehensive guide will delve into the foundational principles of Cognitive Behavioural Therapy, explaining the intricate connection between our thoughts, emotions, and actions. We will explore the essential toolkit of CBT techniques, illustrating how they are applied to address common mental health challenges such as depression, anxiety, and Obsessive-Compulsive Disorder (OCD). Furthermore, you will gain insight into what to expect during therapy sessions, the crucial role of your therapist, and the importance of practice between sessions. We will also highlight the robust evidence base supporting CBT's effectiveness and discuss how it is shaping the future of mental healthcare globally, with the market projected to reach $34.25 billion by 2034.
Addressing Stigma: Embracing Mental Well-being
The journey towards mental well-being often begins with overcoming stigma. For too long, mental health struggles have been shrouded in silence and misunderstanding. CBT offers a beacon of hope by providing a tangible, skills-based approach that emphasizes proactive self-management. Recognizing that mental health conditions are treatable, just like physical ailments, is the first step toward embracing support. As more than a third of UK adults have sought help from a counsellor or psychotherapist at some point, the acceptance of professional support is growing. This guide is designed to empower you with knowledge, fostering an understanding that seeking help is a sign of strength, not weakness.
What is Cognitive Behavioural Therapy (CBT)? Unpacking the Core Principles
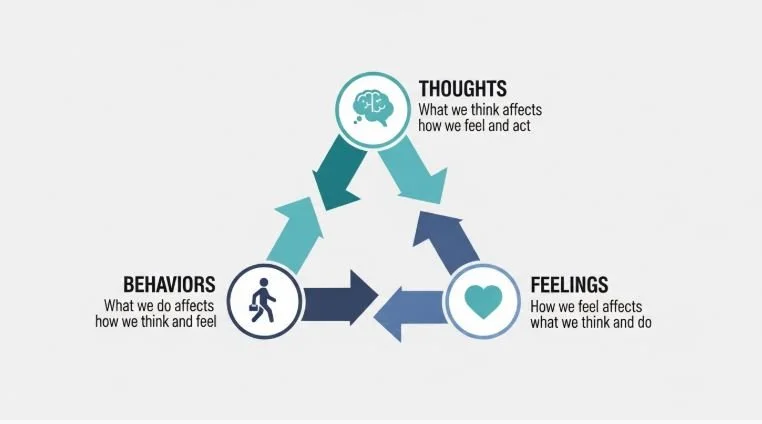
The core principle of CBT is the 'Cognitive Triangle,' which illustrates the interconnected relationship between our thoughts, feelings, and behaviors.
Cognitive Behavioural Therapy, commonly known as CBT, is a type of psychotherapy that is highly effective in treating a wide range of mental health conditions. It is a practical, goal-oriented form of therapy that focuses on developing coping strategies for specific problems. CBT works by breaking down overwhelming problems into smaller parts, making them easier to manage.
Defining CBT: The Interconnectedness of Thoughts, Feelings, and Behaviors
At its heart, CBT is built on the principle that our thoughts, feelings, and behaviors are interconnected and influence each other. It posits that it's not external events themselves that cause distress, but rather our interpretations and thoughts about these events. For instance, a negative thought about an upcoming social event might trigger feelings of anxiety and lead to avoidance behaviors, such as declining the invitation. Similarly, engaging in behaviors like exercise can positively impact mood and reduce feelings of depression. Understanding this triad—thoughts, feelings, and behaviors—is central to the therapeutic process.
The Foundational Philosophy: Why CBT Works
The foundational philosophy of CBT is rooted in its present-focused and problem-solving approach. Unlike some other forms of psychotherapy that may delve extensively into past experiences, CBT primarily concentrates on current issues and how to manage them effectively. It is collaborative, meaning the therapist and client work together as a team to identify problems and develop strategies. This approach empowers individuals by teaching them practical skills to become their own therapists, leading to lasting change and reduced relapse rates. Research indicates that response rates for CBT can range from 50-75% for common conditions, often with lower relapse rates than medication alone .
The Difference Between Cognitive Therapy and Behavioral Therapy (and how they combine)
Cognitive Behavioural Therapy is a synthesis of two distinct yet complementary therapeutic approaches: cognitive therapy and behavioral therapy. Cognitive therapy focuses on identifying and challenging negative or unhelpful thought patterns that contribute to distress. It helps individuals recognize cognitive distortions—such as black-and-white thinking or overgeneralization—and replace them with more balanced and realistic perspectives.
Behavioral therapy, on the other hand, emphasizes changing maladaptive behaviors. Techniques like exposure therapy and behavioral activation are used to help individuals confront fears, increase engagement in rewarding activities, and develop healthier routines. CBT integrates these two modalities, recognizing that changing thoughts can influence behaviors, and conversely, changing behaviors can impact thoughts and feelings. This synergistic approach allows for a comprehensive treatment plan that addresses the multifaceted nature of mental health challenges. CBT and Guided Self Help together account for a significant portion of therapy within NHS Talking Therapies, demonstrating their prominence in mental health services.
The CBT Toolkit: Essential Techniques for Change
CBT employs a variety of evidence-based techniques designed to help individuals understand and modify their thought patterns and behaviors. These tools are practical, actionable, and tailored to individual needs.
Identifying Automatic Thoughts and Cognitive Distortions
The first step in the CBT process often involves learning to identify automatic thoughts—rapid, often unconscious thoughts that pop into our minds. These can be fleeting but significantly influence our emotions and actions. Alongside these, clients learn to recognize cognitive distortions, which are systematic errors in thinking that lead to negative interpretations. Common distortions include catastrophizing (expecting the worst), personalization (taking responsibility for events outside one's control), and filtering (focusing only on the negative aspects of a situation). Becoming aware of these patterns is crucial for challenging them.
Cognitive Restructuring: Challenging and Changing Thought Patterns
Once automatic thoughts and cognitive distortions are identified, the process of cognitive restructuring begins. This involves actively questioning the validity of these negative thoughts. Clients are encouraged to gather evidence for and against their beliefs, consider alternative explanations, and develop more balanced and realistic perspectives. For example, instead of thinking "I'm a complete failure," a restructured thought might be, "I made a mistake, but I can learn from it and try again." This process helps to reduce the emotional intensity associated with negative thoughts and promotes a more positive outlook.
Behavioral Activation: Re-engaging with Life and Purpose
For individuals experiencing depression or low motivation, behavioral activation is a key technique. It focuses on gradually increasing engagement in meaningful and enjoyable activities. The underlying principle is that a lack of activity can perpetuate low mood and withdrawal. By scheduling and participating in activities—even small ones—clients can experience a sense of accomplishment, pleasure, and increased social connection, which in turn can lift their mood. This technique is particularly useful for overcoming the inertia that often accompanies depression.
Exposure Therapy: Gradually Facing Fears and Anxieties
Exposure therapy is a powerful technique, especially for treating anxiety disorders and phobias. It involves gradually and systematically exposing individuals to feared objects, situations, or thoughts in a safe and controlled environment. The goal is to reduce the fear response through repeated exposure, demonstrating that the feared outcome is unlikely or manageable. This process helps to break the cycle of avoidance that often maintains anxiety. For instance, someone with a fear of flying might start by looking at pictures of planes, then watching videos, and eventually taking short flights.
Behavioral Experiments: Testing Beliefs Through Action
Behavioral experiments are designed to test the validity of specific beliefs or assumptions through direct experience. Similar to cognitive restructuring, but action-oriented, these experiments involve creating situations to gather evidence about a particular thought or prediction. For example, someone who believes "If I ask for help, people will think I'm incompetent" might conduct an experiment by asking a colleague for assistance and observing their actual reaction. The results of these experiments can provide powerful disconfirming evidence against negative beliefs.
Relaxation and Mindfulness Techniques Integrated into CBT
CBT often incorporates relaxation and mindfulness techniques to help manage stress, anxiety, and emotional distress. Relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, and guided imagery, help to calm the nervous system. Mindfulness, the practice of paying attention to the present moment without judgment, can help individuals become more aware of their thoughts and feelings without getting overwhelmed by them. These practices enhance self-awareness and provide immediate coping mechanisms for managing difficult emotional states.
CBT in Practice: How It Helps Specific Conditions
The versatility of CBT makes it an effective treatment for a wide range of mental health conditions, providing tailored strategies for diverse challenges.
For Anxiety Disorders: Generalized Anxiety, Social Anxiety, and Panic
CBT is a leading treatment for various anxiety disorders. For generalized anxiety disorder, it helps individuals identify and challenge excessive worry and catastrophic thinking. In social anxiety, it focuses on challenging negative self-perceptions and fear of judgment, often incorporating social skills training and exposure. For panic disorder, CBT helps individuals understand the physical sensations of panic, challenge catastrophic beliefs about these sensations, and use relaxation techniques to manage acute attacks. A 2023 meta-analysis found CBT to have moderate to large effects compared to control conditions for anxiety
For Depression: Overcoming Low Mood and Loss of Interest
CBT is highly effective for depression by addressing negative thought patterns and behaviors that contribute to low mood and anhedonia (loss of interest or pleasure). Cognitive restructuring helps individuals challenge self-critical thoughts, feelings of hopelessness, and pessimism. Behavioral activation encourages them to re-engage in activities they once enjoyed or find fulfilling, counteracting withdrawal and apathy. This dual focus on thoughts and actions can significantly improve mood and restore a sense of purpose.
For Obsessive-Compulsive Disorder (OCD): Managing Intrusive Thoughts and Compulsions
CBT, particularly a form known as Exposure and Response Prevention (ERP), is considered the gold standard treatment for OCD. ERP involves exposing individuals to their feared obsessions (e.g., thoughts about contamination) while preventing them from performing their usual compulsive rituals (e.g., excessive handwashing). This process helps individuals learn that they can tolerate the discomfort of their obsessions without resorting to compulsions, thereby reducing the power of OCD. Research indicates that 75% of people with OCD are significantly helped by CBT, with some services reporting recovery rates of up to 80% [Source 9].
For Posttraumatic Stress Disorder (PTSD) and Trauma
Specialized forms of CBT, such as Trauma-Focused CBT (TF-CBT) and Eye Movement Desensitization and Reprocessing (EMDR), are highly effective for PTSD and trauma-related conditions. These therapies help individuals process traumatic memories, reduce avoidance of trauma-related cues, challenge negative beliefs about oneself and the world, and develop coping mechanisms for managing symptoms like flashbacks, nightmares, and hypervigilance.
Beyond the Usual Suspects: CBT for a Wider Range of Challenges
CBT's utility extends beyond the commonly cited conditions. It is also an effective treatment for issues such as phobias, eating disorders, sleep disorders (like insomnia), substance use disorders, chronic pain management, anger management, and relationship problems. Its adaptable nature allows therapists to tailor interventions to address the specific cognitive and behavioral patterns underlying a wide array of mental health conditions and life challenges.
Your Journey Through CBT: What to Expect in Therapy
Embarking on CBT can feel daunting, but understanding the process can make it a more manageable and rewarding experience. The journey is collaborative, empowering, and focused on equipping you with lifelong skills.
Finding the Right Mental Health Professional: Therapists, Psychologists, Counselors, and Psychiatrists
When seeking CBT, you might encounter various professionals, including psychologists, licensed clinical social workers (LCSWs), licensed professional counselors (LPCs), and psychiatrists. Psychologists often have extensive training in CBT and psychological assessment. Therapists and counselors provide talk therapy and can be trained in CBT techniques. Psychiatrists are medical doctors who can diagnose mental health conditions, prescribe medication, and may also offer CBT. The most crucial factor is finding a qualified therapist who is experienced in CBT and with whom you feel comfortable and can build a strong therapeutic alliance. More than a third of UK adults have sought help from a counsellor or psychotherapist, highlighting the growing accessibility of these services BACP, 2025.
The Initial Assessment Phase: Understanding Your Needs and Goals
The initial sessions with your therapist will typically involve a thorough assessment. The therapist will ask about your symptoms, their history, your current life situation, and your personal goals for therapy. This phase is crucial for the therapist to understand your unique challenges and for you to feel comfortable sharing. Together, you will identify specific problems you want to work on and establish clear, achievable goals for your treatment.
Collaborative Treatment Planning: You as the Client in Charge
A hallmark of CBT is its collaborative nature. Your therapist will not simply dictate a treatment plan; instead, you will work together to develop one. This involves discussing which CBT techniques seem most appropriate for your situation and agreeing on the strategies you will employ. This ensures that you are an active participant in your healing process, feeling a sense of ownership and empowerment over your treatment.
What Happens in Therapy Sessions: Structure and Engagement
CBT therapy sessions are typically structured and focused. Each session usually begins with a brief review of your week and any "homework" you completed. The therapist will then work with you on specific skills or issues, often introducing new techniques or reinforcing previously learned ones. Sessions are interactive, involving discussions, exercises, and planning for the week ahead. The therapist's role is to guide, teach, and support you, while your role is to actively engage, practice, and apply what you learn.
The Importance of "Homework" and Practice Between Sessions
A key component of CBT's effectiveness is the practice of skills learned in therapy between sessions. This "homework" can involve various tasks, such as monitoring your thoughts, practicing relaxation techniques, engaging in specific behaviors, or completing worksheets. These assignments are not busywork; they are opportunities to apply CBT principles to real-life situations, solidify learning, and accelerate progress. Consistent practice is vital for integrating new coping mechanisms into your daily life and achieving lasting change.
Duration of CBT: Short-Term vs. Long-Term Approaches
CBT is often described as a short-term therapy, typically lasting between 12 to 20 sessions for common issues like anxiety and depression. However, the duration can vary significantly depending on the complexity and severity of the presenting problems. Some individuals may see significant improvement in as few as four to six sessions, while others may benefit from more extended treatment. The focus is on equipping you with skills to manage your mental health effectively long-term, rather than creating dependency on therapy. CBT is generally understood as a therapy lasting weeks and months, rather than years [Source 9].
When to Consider Ending Therapy or Seeking Further Support
The decision to end therapy is usually made collaboratively with your therapist. Generally, it's time to consider ending when you have met your treatment goals, feel confident in your ability to manage challenges independently, and have developed robust coping strategies. You might also choose to continue therapy if new issues arise or if you wish to deepen your understanding and skills. It's also important to know when to seek immediate professional help if you experience a crisis or have thoughts of harming yourself or others.
The Evidence Base: Why CBT is a Gold Standard Treatment
The widespread adoption and recommendation of CBT are not accidental; they are firmly rooted in a substantial body of scientific evidence demonstrating its efficacy and effectiveness.
Research and Effectiveness
Numerous studies, meta-analyses, and systematic reviews have consistently shown CBT to be a highly effective treatment for a wide range of mental health conditions. Its effectiveness has been established across diverse populations, settings, and delivery methods, including face-to-face, group therapy, and digital platforms. A 2023 meta-analysis of 409 trials, for instance, found CBT to have moderate to large effects compared to control conditions for depression NIH, 2023. This robust evidence base solidifies CBT's status as a "gold standard" treatment for many psychological difficulties.
Empowering Clients for Long-Term Well-being
Beyond symptom reduction, a significant strength of CBT lies in its ability to empower individuals with self-management skills. By teaching clients how to identify and challenge unhelpful thoughts and behaviors, CBT equips them to navigate future challenges independently. This focus on skill-building contributes to lower relapse rates compared to treatments that do not emphasize active client participation and skill acquisition. The goal is not just temporary relief but sustainable well-being and resilience.
Conclusion: Embracing Your Path to Change with CBT
Cognitive Behavioural Therapy (CBT) offers a powerful, evidence-based framework for understanding and transforming the intricate interplay between our thoughts, feelings, and behaviors. Its structured approach, focus on practical techniques, and emphasis on client empowerment make it an invaluable tool for navigating a wide array of mental health conditions, from anxiety and depression to OCD and beyond. By demystifying the therapeutic process, highlighting the importance of collaboration with a qualified therapist, and underscoring the role of practice through "homework," this guide aims to equip you with the knowledge to consider CBT as a viable path toward lasting mental well-being.
The growing global acceptance and integration of CBT, as evidenced by its market expansion and widespread use in healthcare systems, underscore its profound impact. Remember, seeking support is a courageous step. CBT provides not just a treatment but a comprehensive strategy for building resilience and fostering a more balanced, fulfilling life. If you are struggling, consider exploring CBT as a means to gain greater control over your mental health and embark on your journey towards lasting change.